A recently trial REVASCAT (NEJM 17 April 2015), has been published about the usefulness of recanalization by SOLITAIRE device for patients with large vessel occlusion and moderate to severe clinical (NIH> 6). Thrombectomy vs best medical treatment (thrombolysis if less than 4.5 hours, anticoagulation if he was with it) with 1: 1 randomization.
Enlace: clickar NEJM REVACAT 2015
Patients who take less than 8 hours of a major vessel occlusion (ACM M1 segment, terminal carotid occlusion or occlusion in tandem) were included in the study. In turn should have a TAC with an image that demonstrated significant “vital” tissue (mismatch) despite symptoms (scale ASPECTS> 6). While a perfusion image was not required to corroborate that was non-injured tissue its use was recommended.
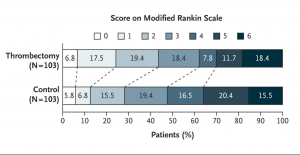
In the thrombectomy group applied the favorable results of functional independence is increased by two compared to best medical treatment group (44% vs 27%). However the mortality was higher, although not significant in thrombectomy group.
They involved more than 200 patients and is an exclusively national study. It has lasted more than two years and although initially planned more than 800 patients (this would have exceeded last for more than six years), the emergence of positive results from other studies thrombectomy has precipitated its end recruitment (December 2014). His goal was main demonstration of efficacy in patients with good functional status at third month (Rankin scale 0-2) and therefore has been presented recently their results (April 17, 2015). Excellent results in the intervention group confirms the usefulness and safety of this technique, with few cases of bleeding or complications.
As curious information highlights the higher mortality in interventional group than other recently published studies of thrombectomy (Mr. Clean, NEJM November 2014 and ESCAPE and EXTEND IA, NEJM February 2015 and April 2015 SWIFT-PRIME) which was contrary and even decreasing significantly lower to the half. Possibly made as patients that could include up to 8 hours even non-thrombolyzed or prior anticoagulant treatment in medical group, interventional use different techniques or intervention times greater problems could justify this.
Another point to note is the important and significant but discreet achieve functional independence at three months results (Rankin 0-2 at the 90 days intervention 44% vs. 24% in better medical treatment) when compared with previous or recent studies the hows SWIFT-PRIME (Link NEJM 2015: 17 April 2015). Possibly the criteria for patient selection, the start time of greater population and different treatments may justify this 10% difference with other studies or previous series.
The other curiosity of REVASCAT trial is that patients accept up to 8 hours (other studies up to 6 or 12 hours) tests justified infusion (over 90% was randomized according to TAC and few gold-standard studies which is the RM). In addition many patients were not always thrombolysis with rtPA previously (accepted or postoperative patient morbidity or prior anticoagulant could not manage rtPA) contributed to these differences.
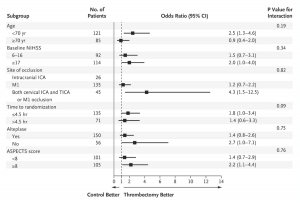
This would justify the results that managed to reach the end-point of functional independence at three months (Rankin 0-2) to the minimum but enough signfication with 200 patients. However it is unlikely that more patients had achieved significantly reduce mortality and seems inherent in the selection criteria of the study.
In addition to differential mortality data with other studies published recently in this year is the lack of apparent utility of these procedures in very elderly patients. However in previous trials this subgroup is the most benefited results, however REVASCAT seems to be pointless, possibly due to a judicious choice without excessive morbidity of these patients and therefore a program of adequate rehabilitation to get good functional recovery by the 90day. Also like other subgroups could receive previous thrombolysis to thrombectomy, unlike those published in previous studies, it is where the interventional treatment had worse outcomes curiously (without being significant).
This contrasts with the feeling and result set of most centers, including ours where these procedures are performed in these treatments greatly reduce the mortality. Such data can be analyzed by checking the Department of Community Health Register (SONIIA) where all endovascular treatments performed in recent years are recorded. This log validate this data has served as control to assess patients excluded from the study and assess possible selection bias.
Despite being already the fifth and final study thrombectomy serves to give consistency and thrombectomy as evidence of effective treatment in large vessel occlusions and moderate to severe clinical when performed by experienced teams. Besides we thought is the first study that could be compared with other patient non-randomized according to SONIIA register.
Recent results presented in 2016 long-term follow-up shows that the benefit of interventionism remains beyond the first year with decreased mortality in interventional arm.
However the percentage of severe stroke that received this treatment represents only 10% of strokes and other treatments such as thrombolysis applies to more than 40% of all ischemic strokes. It will be important to improve delivery times for this last treatment given the large number of community centers-hospitals where it is applied.
In the four largest national hospitals that participated in the Bellvitge, Clinic, Vall d’Hebron and Can Ruti angiography study were available to perform the study and listed as participating centers. However community stroke centers where thrombolysis was performed send us patients when thrombolyisis failed . These centers for evaluation were Hospital Joan XXIII, H.Tortosa Cinta Verge , H. Josep Trueta, H. Arnau de Lleida. And in turn primary stroke hospitals (aided with telestroke) that referred patients to our comprehensive stroke center for review: H. Mora d’Ebre, Figuere H., H. Mataró, H. Tremp, H. Granollers, Vic H., H. San Camil, H. Vilafaranca H. Igualada, H. Moises Broggi.
Following these excellent results it seems obvious that community-primary centers far more 1h- 1h 30 min away from comprehensive stroke centers where usually performed thrombectomy, and if they treat a large numbers of patients with stroke, could consider the establishment of standard treatment thrombectomy standard. While it might initially be difficult to cover 24 hours a day in these new centers given the low number of patients, a new start could be treat patient during business hour/ work-days.
Link: www.nejm.org/doi/full/10.1056/NEJMoa1503780
I refer you to the NEJM editorial of April 17 which justify the changes that have occurred in recent years and of which we are all aware they have contributed to results of these trials. Click here: EDITORIAL
P. Cardona. Co-investigator REVASCAT.