In this section you can check all news and udpate of main studies thatn demonstrated useful of thrombectomy to treat acute stroke.
THROMBECTOMY EXCLUSION CRITERIA:
– Rankin in baseline> 2 (the Rankin 3 could be accepted if this limitation is due to osteoarticular disease, neither comorbidity nor cognitive impairment)
– Patient> 85 years. (Between 80-85 whenever this small infarct or early involvement in neuroimaging, baseline Rankin 0-1 and few comorbidity).
– NIH 30 should be prioritized evaluation of neuroimaging test due to the sedation or intubation.
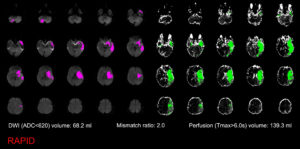
– More than 8 hours duration since onset time, and is already established infarction without viable tissue present in multimodal techniques (CT or MRI perfusion perfusion). EVEN WITH SMALL CORE INFARCT is recommended thrombectomy enrolled in clinic trials because there is no solid evidence of efficacy in patients over 8 hours of evolution (IIB. NEW)
– Platelets less than 30,000
– Time coagulation INR> 3 or APTT> 2.5 and it is impossible to correct.
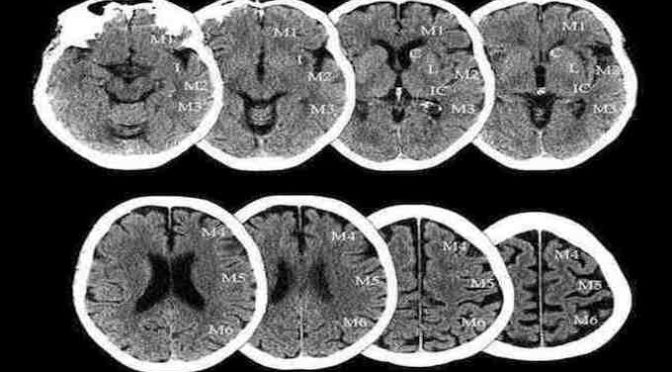
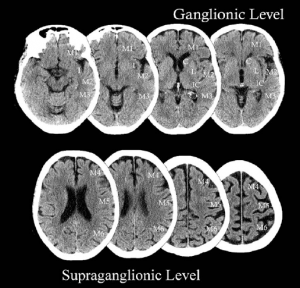
– Recent Stroke with size of more than 1/3 MCA territory (ASPECTscore <7) or massive vertebrobasilar (full involvement in neuroimaging section of stem at a level of 50% or more at different levels (mesencephalon-protuberance-bulb). In case of doubt the performance of multiparametric imaging. (MRI, CT perfusion) enable evaluate infarct penumbra areas. NEW. LOWER LIMIT ASPECTS IT WILL BE 6 (ASPECTS SCORE 0-5 IS NOT RECOMMENDED)
– Bleeding in the hemisphere or in the territory of the same vessel to be treated. (A remote hemorrhagic involvement could not be a contraindication if presented clinical and radiological stability).
– Distal vessel occlusion taht prevent catheter accessibility. NEW RECOMMENDATION 2016: M2 is not recommended because there is no proof, however, in some of the randomized studies included some of these vessels, so most groups agree to treat NIH M2 with high (> 8-10).
– Severe hemodynamic instability, organ failure or other criteria which the physician considers that the risk outweighs the benefit of this treatment.
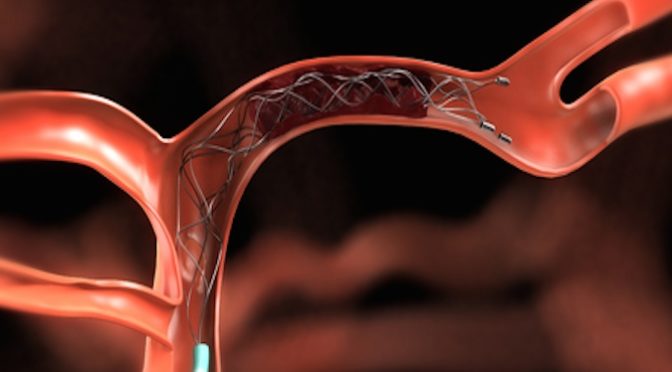
– NEW RECOMMENDATION: It is recommended to use devices other than Solitaire or stent-Trevo Retriever. However it may occasionally use different type systems Penumbra (latest models) or situation given anatomy. (Devices like MERCI or Penumbra is not recommended because of its low percentage of recanalization in different studies IIB)





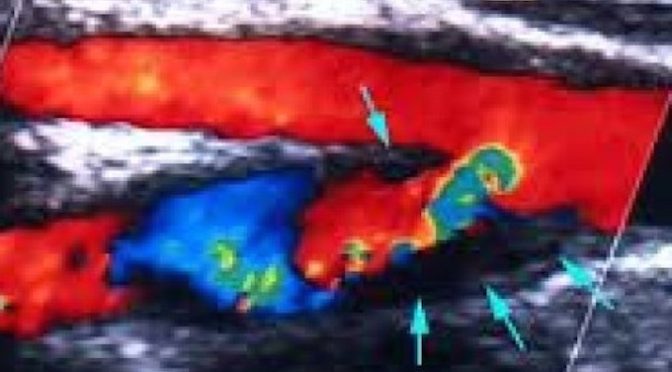
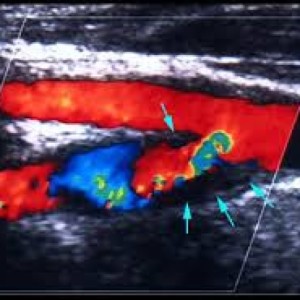 Criterias of stenosis, trick and pitfalls and finding after ultrasound test of carotid or
Criterias of stenosis, trick and pitfalls and finding after ultrasound test of carotid or